In this article, I’m going to provide you with an in-depth review of the similarities and differences of Subutex vs Suboxone. My knowledge and experience on these subjects come from a well-rounded background.
First, I was an opiate addict, and I used both Suboxone and methadone to get off opiates in the past.
Next, I worked as a counselor at an Opiate Treatment Program (OTP) that specializes in Medication-Assisted Treatment (MAT). If they qualified based on a screening with an Intake Specialist (me), our patients could either be placed on methadone, Suboxone, Subutex, or Vivitrol.
90% of my patients were on either Suboxone or methadone, and Medication-Assisted Therapy was my specialty and passion.
Finally, I quit the counseling profession, then went on to become an Opiate Recovery Coach, Blogger, Author, and Speaker…all on the subject of Opiate Detox & Recovery…and I’ve been doing this for over three years now.
You can read my full story here.
Okay…so enough about me.
I simply wanted you to know that I’m not just some writer that studies a topic and then writes an article on it.
I’ve actually lived this, and have been on both sides of the treatment world, as an opiate addict needing help, and as an Opiate Addiction Specialist that helps others.
Coaching and blogging about opiate recovery methods (including Subutex vs Suboxone) is my Life’s Purpose and Mission.
Table of Contents
Subutex vs Suboxone – Overview
Like I stated in the introduction, in this article, I’ll be covering the similarities and differences of Subutex vs Suboxone.
Both of these are very effective and proven opiate replacement medications used in the treatment of opioid dependence.
As an Intake Counselor at an OTP, whenever I performed screenings (in person or on the phone), often times I was asked to explain the difference between Subutex vs Suboxone.
Choosing a powerful opioid replacement medication is a BIG decision.
Thus, I took my time with new and potential admits making sure they understood the similarities and differences, as well as the pros and cons of Subutex vs Suboxone.
Suboxone and Subutex Hit the Scene
On October 8th, 2002, the FDA announced the approval of Subutex and Suboxone tablets for the treatment of opioid dependence. Subutex and Suboxone also became the first narcotic drugs available for the treatment of opioid dependence that could be prescribed in an office setting under the Drug Addiction Treatment Act (DATA) of 2000.
As a result of these changes in policy, many opiate-dependent individuals were now able to be treated with Subutex and Suboxone.
Some people chose to enroll in OTP’s and received Suboxone in an outpatient treatment setting (which includes counseling), while others opted for treatment under the care of a private physician.
All over the nation, people were getting the help they really needed, and for over 15 years now, Subutex and Suboxone have continued to save lives, careers, homes, marriages, families, and much more.
Opiate Addiction 101
Before I discuss the similarities and differences of Subutex vs Suboxone, I believe it’s important for you to have at least a basic understanding of “Opiate Addiction 101.”
So here’s a brief overview of how it all works in the body…
Opiates are drugs that are derived from the opium poppy plant. Opioids are synthetic or natural drugs that do not originate from the opium poppy plant, however, they still bind to the same opioid receptors in the brain and body that opiates bind to, resulting in the same types of effects.
Despite all of the associated negative aspects (addiction, overdose, crime, etc.), prescription opiates still have a positive intent. They are commonly prescribed for the treatment of moderate to severe pain.
These drugs, along with heroin, attach to specific proteins called opioid receptors, which are located on nerve cells in the brain, spinal cord, GI tract, and other organs.
Once these drugs attach to the opioid receptors, their effects come on, which include, but are not limited to:
- Pain Relief
- Euphoria
- Sedation
- Constipation
- Nausea
As human beings, we already have an endogenous painkilling system that is capable of producing pain relief, sedation, and euphoria.
This natural pain relief system is activated when we exercise, eat certain foods (e.g. dark chocolate and chili peppers), or perform other activities.
For example, imagine a man who has just run five miles along the beach.
As a result of this intense physical exertion, his body naturally produces its own opioid chemicals, known as endorphins and enkephalins, thus reducing pain, and promoting euphoria naturally (“runners high”).
Tolerance and Dependence
We already produce natural opioid chemicals (endorphins/enkephalins) in the precise amounts our bodies were designed to handle. The problem arises when an individual has been using an opioid drug for a period of time.
After prolonged use of opioid drugs, the production of endogenous opioids is inhibited, which accounts in part for the withdrawal syndrome that results from the immediate cessation of the drug.
The continuous use of opioids overrides our natural ability to produce endorphins and enkephalins.
The brain comes to rely on the drugs to create these neurotransmitters.
When a person stops using the opioid drug, the brain doesn’t start creating these endogenous opioids right away. It short-circuits, leading to withdrawal symptoms, and deteriorating psychological function.
Whether an individual is abusing opioids or even taking them as prescribed by a physician, the continued use quickly leads to tolerance. Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a decrease of the drug’s effects over time.
If an individual continues using opioids after a tolerance has been established, they will eventually develop a physiological dependence.
Dependence develops when the neurons adapt to the repeated drug exposure and only function normally in the presence of the drug.

Opiate Withdrawal Syndrome
When a dependent individual abruptly stops taking opioids (leading opioid-blood concentration to fall below the required level), the now opioid-tolerant central nervous system (CNS) goes haywire. With no inhibitive stimulation to satisfy receptors, the pathways of the CNS fire signals strenuously, performing at a level much higher than pre-dependence levels.
Now the locus coeruleus responds by triggering the autonomic fight or flight response. What results is known as the opioid withdrawal syndrome, and it’s one of the most horrific experiences an individual could even go through.
Physical opiate withdrawal symptoms include:
- Diarrhea
- Achy Muscles and Limbs
- Gastrointestinal (GI) Distress
- Nausea
- Hot and Cold Sweats and Chills
- Goosebumps
- Vomiting
- Teary Eyes
- A Runny Nose
- Sneezing
- Fatigue
- Restless Leg Syndrome (RLS)
Mental/Emotional opiate withdrawal symptoms include:
- Anxiety
- Insomnia
- Depression
- Panic Attacks
- Social Anxiety
- Anhedonia (Inability to Feel Pleasure)
- Suicidal Thoughts
- Stress
- Inability to Relax
- Lack of Motivation
- Fear
As you can see, there are plenty of opiate withdrawal symptoms that can afflict you while lowering your dosage too fast, or coming off opioids cold turkey. The really awful aspect of opiate withdrawal is that you get hit with a ton of different physical and psychological opiate withdrawal symptoms.
If it were just one or the other, it wouldn’t be near as horrific of an experience.
But alas this isn’t the case.
Opiate withdrawal symptoms are both physical and psychological, and most of the time these symptoms are very severe. Fortunately, you can use medications such as Subutex and Suboxone to eliminate opiate withdrawal symptoms and cravings. Now let’s discuss how these medications work…
Suboxone Overview
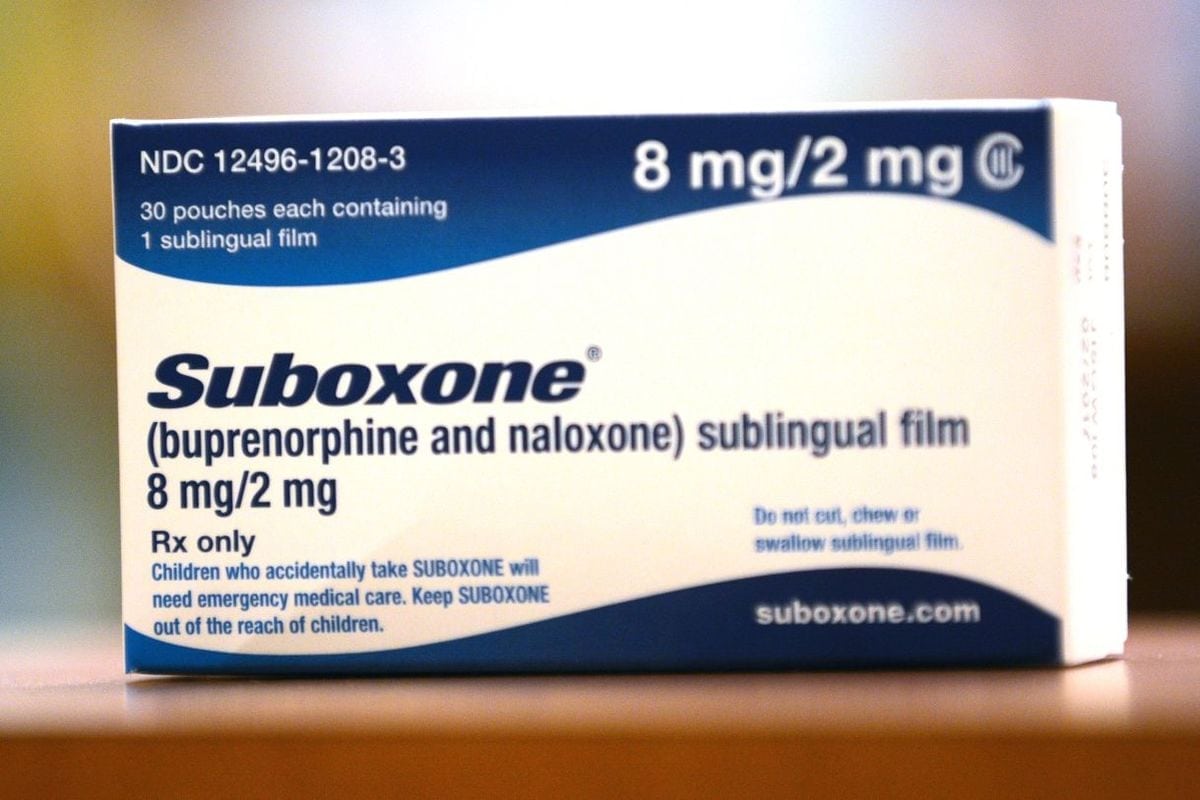
Suboxone is a prescription medication containing buprenorphine and naloxone. Buprenorphine is a controlled substance and semisynthetic opioid derivative of thebaine.
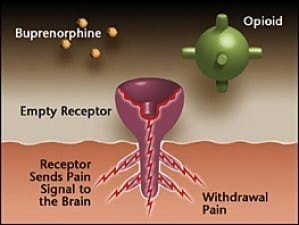
Buprenorphine attaches and binds to the same opioid receptors in the brain and other parts of the body that drugs like heroin, oxycodone, hydrocodone, morphine, and other opioids bind to.
Once it attaches to these receptors, it mimics the effects that opiate drugs produce (though it’s not as powerful).
For this reason, buprenorphine is known as a “partial opioid agonist.”
The other opiate drugs I just mentioned are known as “full opioid agonists,” because they activate the receptors in a stronger and more complete way than buprenorphine. See the illustration below.
Buprenorphine helps opioid-dependent individuals because the daily use of the drug prevents opioid withdrawal symptoms and opioid cravings.
Buprenorphine is very effective at this.
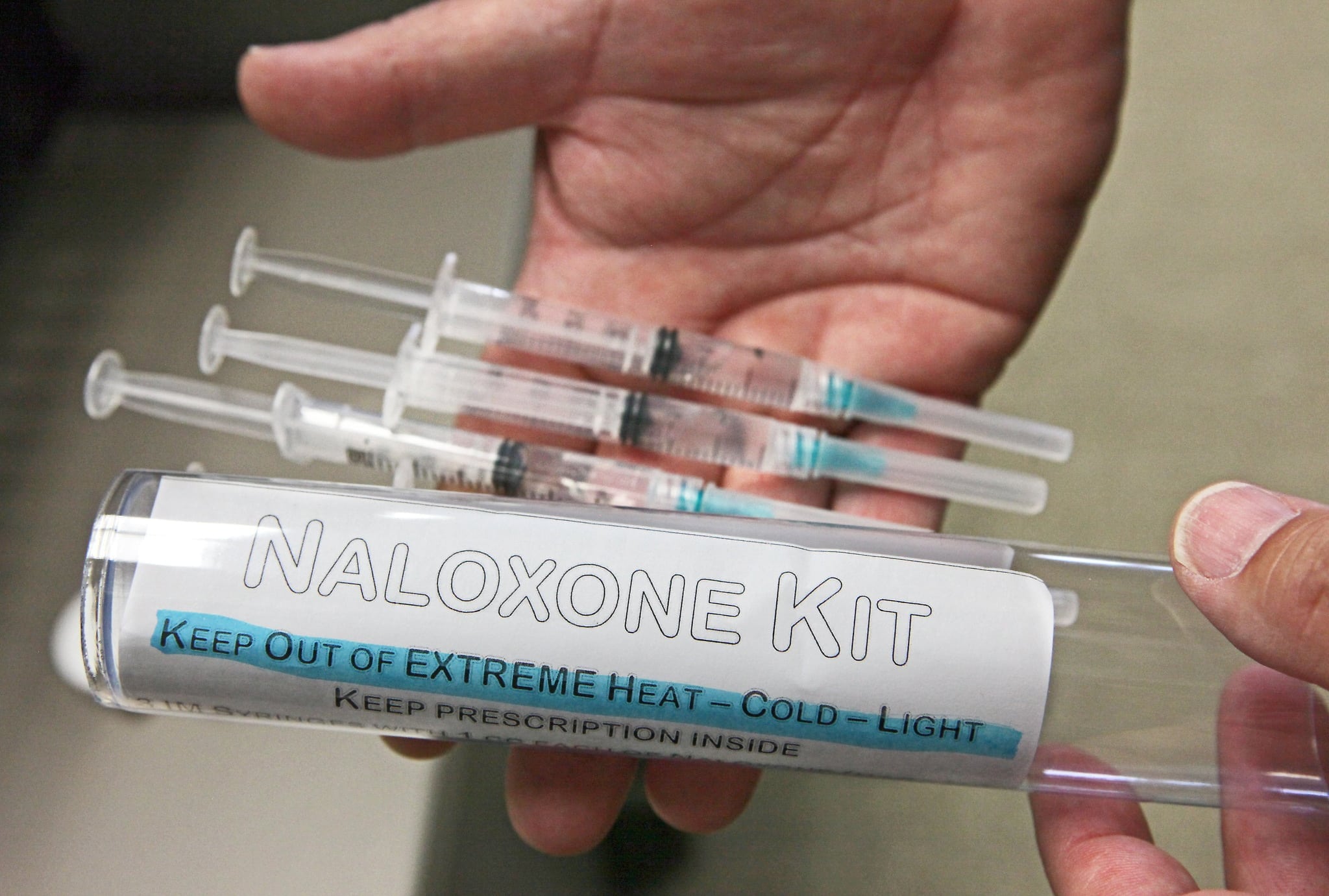
Naloxone is the other compound present in Suboxone.
Naloxone is a pure opioid antagonist. It’s the drug given to people that overdose because an injection of naloxone puts the opioid-user into instant withdrawal, thus saving them from health issues and death.
Naloxone was put into the Suboxone formulation to deter people from injecting it, which would lead to precipitated withdrawal. Taken orally, naloxone isn’t bioavailable. A common misconception is that naloxone blocks the opiates.
This is false.
The truth is that buprenorphine binds so strongly to the opioid receptors that it’s actually the buprenorphine which blocks opioids.
Subutex Overview
Subutex is very similar to Suboxone. Subutex contains buprenorphine but does not contain naloxone. For this reason, it is easier to abuse than Suboxone.
Subutex is harder to get take-home medication from Opiate Treatment Programs because it doesn’t contain the naloxone “abuse-deterrent” drug component. If someone wants to get high on Subutex, they can inject the medication intravenously into their veins, whereas you cannot do that with Suboxone due to Suboxone’s addition of naloxone.
This being said, Subutex is still an extraordinary medication. For responsible adults that are motivated to live a life free of addiction, Subutex can be a true lifesaver. It works very well at eliminating opiate withdrawal symptoms and cravings and has helped a superabundance of individuals over the years.
Subutex vs Suboxone – Key Concepts Breakdown
To further illustrate the comparison of Subutex vs Suboxone, I’ve devised the following 8 key concepts as a simple breakdown for you to see the main differences and similarities of Subutex vs Suboxone.
1. Subutex vs Suboxone Formulation
Subutex is a sublingual pill. Suboxone can be used as a sublingual tablet or film.
2. Subutex vs Suboxone Composition
Subutex contains 100% buprenorphine as the active ingredient. Suboxone contains 80% buprenorphine/20% naloxone.
3. Subutex vs Suboxone Dosage
Both Subutex and Suboxone are typically used in the following dosage range to prevent opioid withdrawal symptoms and cravings: 8 mg to 32 mg per day.
4. Subutex vs Suboxone Accessibility
Suboxone is very easy to obtain take-home medication for outpatient treatment, while Subutex is often less accessible for take-homes at outpatient treatment due to it not containing the naloxone abuse deterrent.
5. Subutex vs Suboxone Price
Subutex is less expensive averaging around $250 – $400 a month or more, while the Suboxone cost is typically a little more, averaging around $350 – $600 a month or more.
Luckily, both Subutex and Suboxone have coupons you can get from your doctor or online that help to offset the cost of these medications.
6. Subutex vs Suboxone Side Effects
Since Subutex and Suboxone have different drug profiles, they also have slightly different potential side effects. Side effects vary from person to person.
Some people get no side effects or very low side effects, while others get some very unpleasant side effects.
Common Subutex Side Effects:
- Drowsiness (or Energy)
- Dizziness
- Constipation
- Headaches
Common Suboxone Side Effects:
- Drowsiness (or Energy)
- Dizziness
- Constipation
- Vomiting
- Sweating
- Dry Mouth
- Nausea
- Lightheadedness
Click here to read the complete list of possible Suboxone side effects, and click here to read the complete list of possible Subutex side effects.
7. Subutex vs Suboxone Abuse Risk
The risk of patients abusing Subutex is much higher than the risk of patients abusing Suboxone. While there is a “ceiling effect” at 32 mg of both medications (meaning using more of the drug will not produce any more opioid effects), Suboxone is less likely to be abused due to the presence of naloxone in the formulation.
Subutex contains only buprenorphine, making it easy to inject intravenously without the risk of a naloxone-precipitated withdrawal syndrome, as is the case with injecting Suboxone.
8. Subutex vs Suboxone Stigma
There is a pretty big stigma associated with using both Subutex and Suboxone, though the stigma associated with using Subutex may be a little worse as it’s seen as less safe than using Suboxone.
Society may look down upon people using either of these medications, though the stigma is still not as bad as it is for people on methadone.
Subutex vs Suboxone – Which One is Right For Me?
Now that you’ve read my in-depth review of the similarities and differences of Subutex vs Suboxone, you may be wondering which medication would be best for you to use.
Additionally, you may have decided that you don’t want to use either of these medications for your opiate recovery. Either way, it’s good to educate yourself on the options available.
Only you and your prescribing doctor together can decide which medication you should start with if you’re going down the “opiate replacement medication road.” It’s also important to note that Subutex and Suboxone are not “silver bullets.” Too many times people just want the medication, but don’t do anything else to change their lives.
The people that have the most success on Subutex and Suboxone also use one or more of the following addiction treatment modalities:
- Individual Counseling
- Group Counseling
- Self-Help Meetings
- Nutrition
- Supplementation
- Personal Development
- Spirituality/Religion
- Meditation
- Exercise
One of my specialties when working with coaching clients is helping them come up with individualized, “holistic” treatment plans that incorporate the whole person (Body, Mind, Spirit).
Although most people don’t hire me to help them get on Subutex or Suboxone, often they reach out to me to become a coaching client after years of being on these medicines and wanting some professional help coming up with a holistic plan to get off medication completely, in the most painless way possible (my specialty).
Subutex vs Suboxone – Final Thoughts
I hope you enjoyed learning about this topic of Subutex vs Suboxone! If you found value from what you read, then you’ll LOVE the Ultimate Opiate Recovery System.
It’s a complete program that teaches you everything you need to know to get off opioid drugs in the most painless and easiest ways imaginable.
I also recently published a brand new article on the newest FDA-approved buprenorphine product, called Sublocade, which is quite impressive! It’s a monthly buprenorphine injection that provides steady levels of buprenorphine daily over the course of one month.
Click here now to read my Sublocade Review article.
And if you have any comments or questions on the topic of Subutex vs Suboxone, please post them in the comment box below. Take care!

















Suboxone saved my life. I’ve been an addict for 15 years over half my life. the last five of my addiction I struggle to get clean trying over and over and just failing every time. The best decision I ever made was to say that I could not do this by myself because it obviously was not going to work so with the help of the medication and lots of counseling and therapy getting back to my core values I am over one year clean. But I could not have focused on my treatment without the withdrawal deterrent and craving deterrent of the Suboxone medication
So I’m having hard time understanding the pre-cip withdrawal.
Does both cause pre-cip withdrawal or is it just the suboxone am not subutex?
I’m battling this, an I can’t seem to ever get that so called allowed 24 hours or more. Please any information will be great
I didn’t realize that a suboxone treatment could help you minimize the withdrawal symptoms that you could potentially experience. This seems like it would be a really good thing because withdrawals would probably be the worst. That way the individual can live a bit more of a normal life and can also recover from their addiction more rapidly.